Stages of Dementia
Alzheimer’s dementia is a terminal illness, but duration of the disease (once detected) can vary from at little as one year to 20. Typically, dementia course is more like several to 12 years. The stages progress more quickly as they advance. Keep in mind that dementia usually starts many years, decades, before it is formally detected in a formal assessment. There are different stage theories with five or more stages, but people differ so much when using multi-stage models that they aren’t reliable ways to describe folks well enough to be used as a diagnostic tool. In other words, there is not enough agreement among health care providers and others using a five-stage model to make it useful. So, we use a simpler three-stage system, like that described by the Alzheimer's Association, is best in talking with family:
First stage dementia (typically lasts 3-6 years), often called mild dementia or early-stage, is marked my mild confusion and forgetfulness like repeating oneself with impaired ADLs like paying bills twice and forgetting to take medicines or neglect of personal hygiene. People have trouble coming up with the right word and may be disorganized at times.
Second stage dementia (last about 2-3 years), called moderate dementia or middle-stage, is marked by pronounced short-term memory deficits and confusion. ADL impairment often results in Assisted Living Facility (ALF) placement. 60% of people in 2nd stage dementia have psychiatric problems like paranoid delusions (someone is stealing my things) with some even show hallucinations.
Third stage dementia, is also called severe dementia or late-stage. Patients at this stage are often in nursing homes, and require full-time assistance and supervision. Vocabulary may be limited to six or fewer words and the patient may fail to recognize family. Mercifully, this stage lasts about 1 year or less, as these patients are targets for opportunistic infections like repeated UTIs or pneumonia.
Mild Cognitive Impairment (MCI)
Suppose someone has a short-term memory problem, but no other cognitive deficits, and/or the problem is not significant enough to interfere with ADLs? They may meet criteria for MCI. If short-term memory was OK, but there was a language problem like a word-finding deficit and/or episodes of confusion, we would call this a non-amnestic MCI. If the biggest complaint is memory difficulty, than that is an amnestic MCI. There may be mood changes like irritability, too.
The American College of Physicians estimates that 20% of people over 70 have MCI. All individuals with Alzheimer’s dementia (and most other types) go through a period of MCI before it progresses to full blown dementia. However, not all people with MCI develop Dementia. Dr. Petersen and his colleagues at the Mayo Clinic have studies MCI on a longitudinal basis (over a long term) and discovered that about 50% of MCI patients progress to dementia in four years, and 80% within six years. Knowing a patient has MCI is an important factor in planning (e.g., Medicaid Estate Planning) and engaging in strategies to reduce this heightened risk. Visit the Mayo Clinic’s website for more information about MCI:
Mild Cognitive Impairment - MayoClinic.com.
Here's a visual display of the progression from MCI to Dementia:
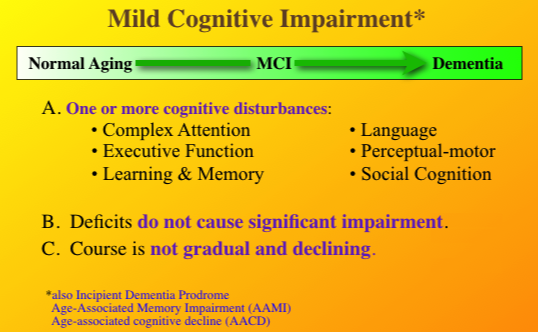
Also note that the technical diagnosis of MCI was changed in October of 2015 and is now called Mild Neurocognitive Disorder. For that matter, the diagnosis of Dementia was also changed to Major Neurocognitive Disorder. You will see most professionals still using the terms MCI and dementia as they are better understood by families, but don't be surprised if you see the new terms in our reports on your insurance bill.