Coronaviruses

Viruses were discovered by the Dutch botanist Martinus Beijerinck in 1898 and he postulated they multiplied and could infect, as a pathogen, living organisms. The picture to the right (public domain, from Wikipdedia) show his working in his laboratory. That same years it was discovered that a virus caused hoof-and-mouth disease which had been killing cattle around Europe. They are much smaller than bacteria (which they often infect) and virus research advanced with the electron microscope developed in the 1930s. Viruses were shown as the cause of rabies and influenza. In 2020 there are 6,828 named virus species; however, there are more than 200,000 unnamed species in the oceans. This NYT article describes the “virosphere” and is summarized below.
Dr. Kuhn is the lead virologist at the Integrated Research Facility at Fort Detrick in Maryland, where a different, infamous military germ lab was shut down in 2017 due to unsafe handling of the Ebola virus. That lab was one of 263 in the US studying weapons grade materials like the neurotoxin ricin, anthrax and a variety of viruses – even the plague. There are hundreds of millions of virus species which mostly infect bacteria; however, a hundreds of millions also infect plants, fungi, animals, and protozoans which are single celled animals that are larger and more complex then bacteria. They cause parasitic diseases, not bacterial or viral infections. Dr. Kuhn estimates that there are at least 100 million virus species that infect just protozoans while some researches suggest the number may be more like 10 trillion. Of relevance are the tiny fraction of viruses, about 250, that infect humans.
It is known that bats are reservoirs for many different viruses. They have developed immunity to them, but they carry viruses which spread easily among them as they live in such close quarters, literally wing-to-wing. In turn, bats spread viruses to other animals which, on occasion, become sick.
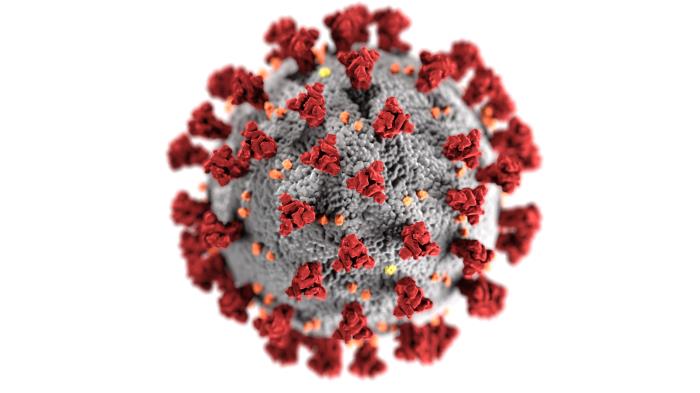
What are Coronaviruses?
It is known that bats are reservoirs for many different viruses. They have developed immunity to them, but they carry viruses which spread easily among them as they live in such close quarters, literally wing-to-wing. In turn, bats spread viruses to other animals which, on occasion, become sick.
What are Coronaviruses?
CNN (02/18/20) reports that coronaviruses are common sources of infection in animals. In rare cases they can be, what scientists call, zoonotic meaning they can be transmitted from animals to humans, according to the US Centers for Disease Control and Prevention (the CDC). Officials do not know what animal may have caused the current outbreak of novel coronavirus in Wuhan, China.

Overall, there are two classes of viruses; those that infect animals (veterinary viruses), and the ones that can infect humans (human viruses). Examples of viruses unique to cats include; Feline Distemper (FD), Herpes (FH) , Leukemia (FeLV), Immunodeficiency Virus (FIV), etc. Feline Coronavirus (FCoV) is contagious to other cats, but not to humans.
Diseases That Pass Between Animals and Humans
Toxoplasmas lives in many cats and can “jump” to humans who handle their litter boxes. This disease is especially problematic to pregnant women, so you may have heard about it. There are at least 15 feline diseases transmittable to humans, but there is no risk that you can get/give COVID-19 from/to your cat or dog.
By the way you can give other diseases to your pets like ringworm, mumps and the flu. It is thought that some human viruses start in bats and/or other animals that live in close proximity like pigs; think of swine flu. In very rare occasions, viruses can jump from animals to humans when they are in close contact, like at the exotic animal market in Wuhan, China.
Coronaviruses
Diseases That Pass Between Animals and Humans
Toxoplasmas lives in many cats and can “jump” to humans who handle their litter boxes. This disease is especially problematic to pregnant women, so you may have heard about it. There are at least 15 feline diseases transmittable to humans, but there is no risk that you can get/give COVID-19 from/to your cat or dog.
By the way you can give other diseases to your pets like ringworm, mumps and the flu. It is thought that some human viruses start in bats and/or other animals that live in close proximity like pigs; think of swine flu. In very rare occasions, viruses can jump from animals to humans when they are in close contact, like at the exotic animal market in Wuhan, China.
Coronaviruses
How Long do they Live and Where?
Not much is know about COVID-19 yet, but there are at least 22 studies about how well other human and veterinary viruses can survive and where. Human coronaviruses, such as SARS and MERS, have been found to persist on surfaces – including metal, glass or plastic – for as long as nine days if that surface had not been disinfected, according to research published earlier this month in The Journal of Hospital Infection.
SARS and MERS viruses appear able to live and remain infectious at room temperature on surfaces for up to nine days. By comparison, the measles virus can only live and contaminate a surface for up to two hours. Carly Cassel of ScienceAlert.com reports that some veterinary coronaviruses (which can only infect animals) can live up to 28 days on surfaces. High humidity in the air and cooler temperatures increase the lifespan of viruses. On average coronaviruses live on surfaces for four to five days, depending on the material (wood, paper, glass or plastic). How to disinfect and even make your own disinfectants and hand sanitizer is covered in a later section of this website.
Not much is know about COVID-19 yet, but there are at least 22 studies about how well other human and veterinary viruses can survive and where. Human coronaviruses, such as SARS and MERS, have been found to persist on surfaces – including metal, glass or plastic – for as long as nine days if that surface had not been disinfected, according to research published earlier this month in The Journal of Hospital Infection.
SARS and MERS viruses appear able to live and remain infectious at room temperature on surfaces for up to nine days. By comparison, the measles virus can only live and contaminate a surface for up to two hours. Carly Cassel of ScienceAlert.com reports that some veterinary coronaviruses (which can only infect animals) can live up to 28 days on surfaces. High humidity in the air and cooler temperatures increase the lifespan of viruses. On average coronaviruses live on surfaces for four to five days, depending on the material (wood, paper, glass or plastic). How to disinfect and even make your own disinfectants and hand sanitizer is covered in a later section of this website.

How Bad can a Virus be?
In 1918 a novel (never seen before) influenza outbreak was first seen in an Army barracks in the United States, despite being called the “Spanish Flu.” As a “novel” disease, no one had yet survived it to develop immunity so it spread, sickened and killed. Like everywhere the disease hit Spain, but as Spain was neutral in WWI and not subject to the strict propaganda control in the U.S. and other warring countries to avoid negative news that might weaken the war effort, it reported on its outbreak first and thus became associated with the eponymic disease. The photo above, from the National Archives, shows convalescing flu patients at the U.S. Army Eberts Field facilities outside an overcrowded hospital in Lonoke, Arkansas in 1918.
Contrary to some people’s statements, the people of Spain hated the name “Spanish Flu” which associated them with the pandemic, forever. The war spread the disease, reportedly infecting 40% of the US Navy and over 35% of the Army who carried the disease further around the world. Even President Woodrow Willson is said to have suffered the flu at the Treaty of Versaille as the war ended. No one knows how many people were killed, but up to about 3% of the world’s population may have died from it.
To understand why a “novel” viral infection is important, consider: The problem is that too few people may survive a new disease in order to develop immunity. Once enough people develop immunity, an epidemic is hard to re-kindle in crowded conditions. There is less spread if a certain percentage of people have immunity; this is called the “herd effect” and is well understood by epidemiologists.

This is why you read about how COVID-19 may subside over the summer, but come again as “a wave” only to subside again in a never ending pattern until enough of us sicken and develop immunity. But, that came too late for 90% or more of the indigenous peoples of Mexico and the US in the smallpox pandemic.
Why not just wait out the epidemic in the US until enough of us have herd immunity? Because between 85–95% of us would have to get sick in order to protect the remaining 10–15%. About 16% of the US population is 65 or over as compared to 8% in 1950 (you can see why SS is in trouble as it relies on the income of younger people, which is shrinking, to pay for senior’s retirement). With a disease that kills 8% of people 60 and over (which is about 70% of the US population of 328 million) that means we’d need to tolerate 18 million deaths to get to herd immunity. And, that is just deaths among seniors, not counting additional millions of deaths in people under 60. BTW, it took two centuries until 1980 when the World Health Organization (WHO) finally announced that smallpox had been eradicated in the human population and that was after 80 years of world-wide efforts years to immunize people against the disease.
The difference today is that we can make vaccines in a year or so – but, how many people will sicken and/or die in the meantime? So temporary shelter-in-place rules make sense to reduce illness, and reduce strain on limited resources like our hospitals and healthcare providers – until we call all be vaccinated.
Just What is a “Pandemic”?
The History Channel has a nice description of past pandemics. Whenever a disease becomes extensive across a country it is called an epidemic. When it spreads to other countries, that’s when it becomes a “pandemic.” They earliest major diseases occurred before there would countries, like tuberculosis, malaria, smallpox, influenza and leprosy occurred when people started aggregating in communities, around 10,000 years ago. Trade, wars and travel became more extensive in the last 1,000 years leading to the first pandemics. Since 1990 there have been five pandemics:
- 1918: Spanish Flu
- 1957: Asian Flue
- 1981: HIV/AIDS
- 2002: SARS
- 2019: COVID-19
- Phase 1: A virus in animals has caused no known infections in humans.
- Phase 2: An animal flu virus has caused infection in humans.
- Phase 3: Sporadic cases or small clusters of disease occur in humans. Human-to-human transmission, if any, is insufficient to cause community-level outbreaks.
- Phase 4: The risk for a pandemic is greatly increased but not certain.
- Phase 5: Spread of disease between humans is occurring in more than one country of one WHO region.
- Phase 6: Community-level outbreaks are in at least one additional country in a different WHO region from phase 5. A global pandemic is under way.
Next Page –>